WASHINGTON, D.C. – The U.S. Justice Department announced a historic 2025 National Health Care Fraud Takedown today, Monday, June 30, 2025, at 3:56 PM EDT, targeting 324 defendants, including 96 doctors, nurse practitioners, pharmacists, and other licensed professionals across 50 federal districts and 12 State Attorneys General’s Offices. Reported at 4:15 PM EDT, the operation, which includes significant involvement from Ohio, addresses alleged health care fraud schemes with an intended loss surpassing $14.6 billion, more than doubling the previous record of $6 billion. This unprecedented effort, involving federal and state law enforcement, aims to protect patients and taxpayers from exploitation, with Ohio playing a key role through its Attorney General’s Office.
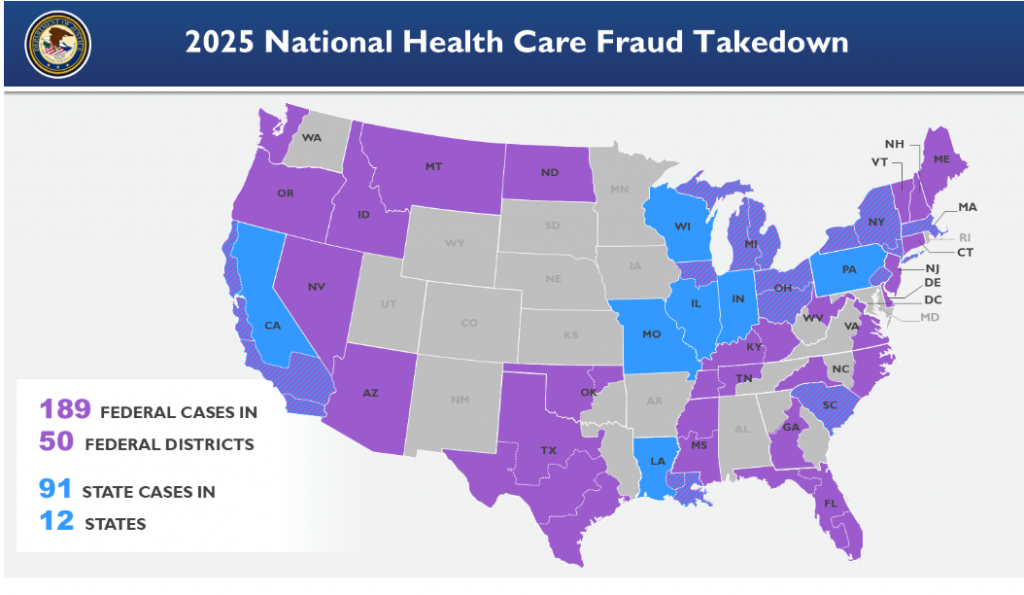
The takedown yielded the seizure of over $245 million in cash, luxury vehicles, cryptocurrency, and assets, showcasing a significant return on fraud enforcement investments. The Centers for Medicare and Medicaid Services (CMS) reported preventing over $4 billion in false claims and suspending or revoking billing privileges for 205 providers ahead of the operation. Civil charges against 20 defendants for $14.2 million in fraud and settlements with 106 defendants totaling $34.3 million were also announced. Ohio’s participation underscores its commitment to this national effort, with the state’s law enforcement agencies collaborating closely with federal partners.
Led by the Justice Department’s Health Care Fraud Unit, in partnership with U.S. Attorneys’ Offices, the Department of Health and Human Services Office of Inspector General (HHS-OIG), the Federal Bureau of Investigation (FBI), and the Drug Enforcement Administration (DEA), the operation tackled diverse schemes. Attorney General Pamela Bondi stated, “This record-setting takedown delivers justice to criminals preying on our vulnerable citizens and stealing from taxpayers. This administration will not tolerate such acts endangering community health and safety.” Ohio Attorney General Dave Yost echoed this sentiment, highlighting the state’s role in protecting its residents from fraud, with the announcement made at 3:58 PM EDT today.
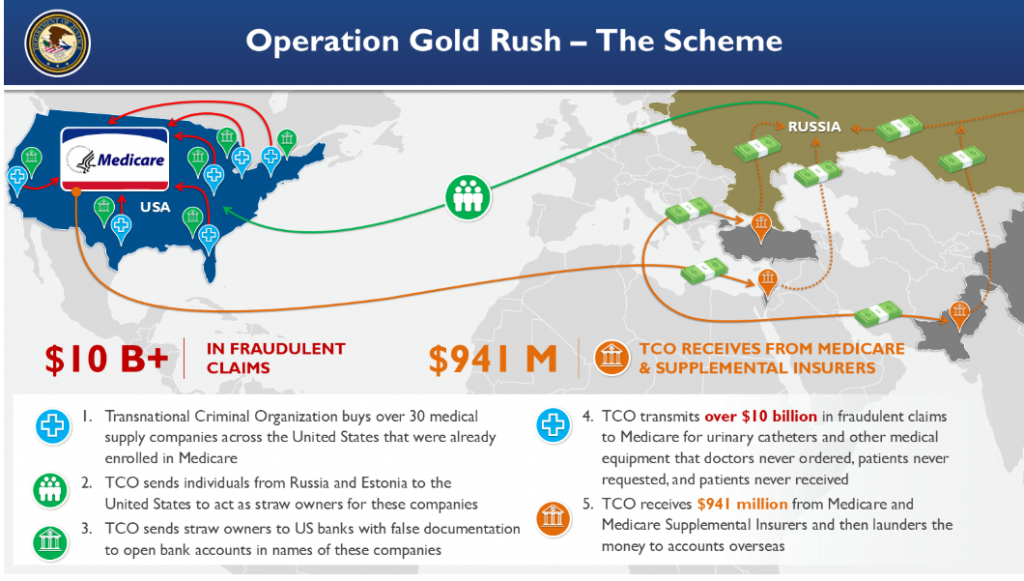
Key cases included Operation Gold Rush, charging 19 defendants with a $10.6 billion Medicare fraud scheme using stolen identities, with $27.7 million seized and $4.41 billion held in escrow for the Medicare trust fund. In Illinois, five defendants faced charges for a $703 million scheme involving AI-generated fake consents, with $44.7 million recovered. A Pakistan-based defendant was charged with a $650 million Arizona Medicaid fraud, pocketing $25 million, including a $2.9 million Dubai home.
Other schemes involved $1.1 billion in fraudulent wound care claims in Arizona and Nevada, targeting elderly hospice patients, and 74 defendants charged with diverting 15 million opioid pills, including a Texas pharmacy distributing 3 million pills. Additionally, 49 defendants were linked to $1.17 billion in telemedicine and genetic testing fraud, while 170 others faced charges for $1.84 billion in various fraudulent claims.
In Ohio, specific cases underscored the state’s significant contribution. In the Northern District of Ohio, Mohammed Ahmad, 39, of Avon, was charged by information with making false statements related to health care matters in connection with a durable medical equipment telemedicine scheme. As alleged, Ahmad, a licensed physician, was paid by a telemedicine company to sign pre-completed orders for durable medical equipment for patients he never treated, resulting in approximately $267,402 in false claims to Medicare, of which $126,643 was paid. The case is being prosecuted by Assistant U.S. Attorneys Chelsea Rice and Erica Barnhill of the U.S. Attorney’s Office for the Northern District of Ohio.
In the Southern District of Ohio, Terry Hill, Jr., 59, of Dayton, was charged by indictment with health care fraud, false statements relating to health care matters, and conspiracy to commit health care fraud for illegally owning and operating Recovery Street Central, a Dayton substance abuse treatment facility. Despite being excluded from Medicare and Medicaid programs in 2021 following a Medicaid fraud conviction, Hill allegedly continued operations, submitting over $4 million in claims to Medicaid for counseling services that were either not provided or violated regulations. The case is being prosecuted by Assistant U.S. Attorney Ken Affeldt and Special Assistant U.S. Attorney Brian Walters, the latter also serving as Senior Assistant Ohio Attorney General for the Ohio Attorney General’s Office – Medicaid Fraud Control Unit.
HHS Secretary Robert F. Kennedy Jr. emphasized, “HHS will aggressively eliminate health care fraud to make care accessible and affordable.” FBI Director Kash Patel added, “With over $13 billion in fraud uncovered, we’re committed to holding accountable those undermining our health care systems.” The operation also launched a Health Care Fraud Data Fusion Center, leveraging AI and analytics to enhance fraud detection, aligning with Executive Order 14243 to reduce silos and boost efficiency.
The Fraud Section, active since 2007, has now charged over 5,400 defendants for $27 billion in fraudulent billing, reinforcing its mission to safeguard health care integrity, with Ohio’s efforts playing a pivotal role.